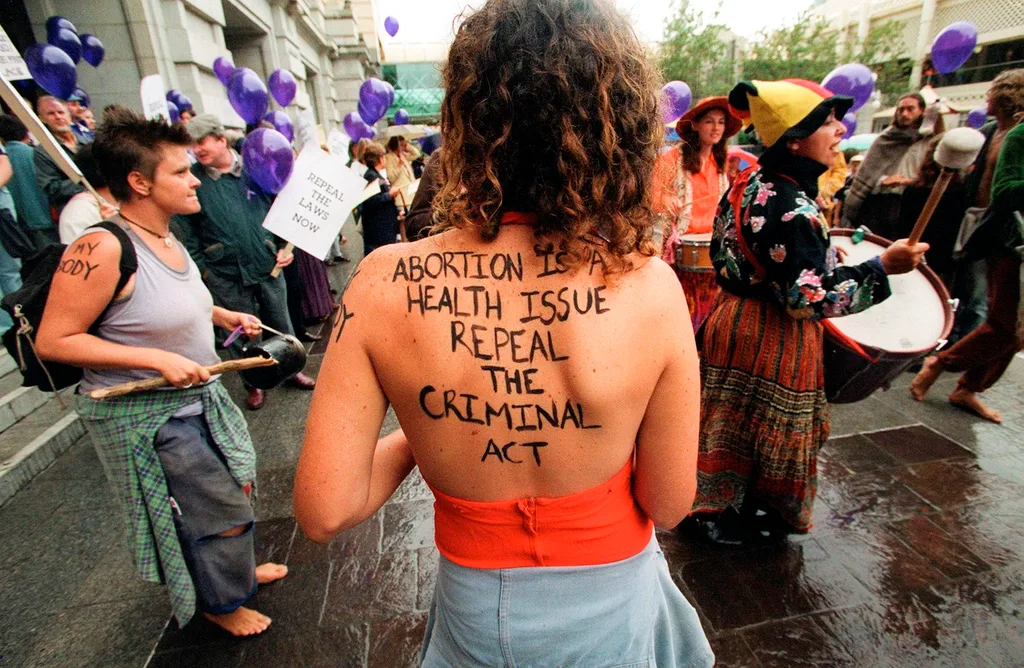
When Queensland passed its historic abortion laws in October, the state erupted in celebration. Crowds cheered outside parliament. Brisbane’s Kurilpa Bridge was illuminated with purple lights to commemorate the moment when women could finally take control of their own bodies and lawfully seek a pregnancy termination without fear of criminal reprisal. And female MPs hugged each other as the bill, which allows women to end their pregnancies up to 22 weeks on request and established safe zones around abortion clinics, passed into law. Witnessing the euphoria, you could be forgiven for thinking Queensland was Australia’s final hold-out state on women’s reproductive rights. Abortion laws nationally, you might assume, have finally limped into the 21st century with equality and safety for all.
Except they haven’t.
In fact, there are still outdated and sexist laws and practices that inhibit women’s reproductive rights all over Australia, not just on abortion but contraception as well. A recent survey published in the Australian and New Zealand Journal of Public Health revealed three-quarters of respondents did not know that abortion is still a criminal offence in NSW, punishable by up to 10 years in jail. In South Australia, two doctors must agree that a woman’s mental or physical health is endangered by a pregnancy before they allow a termination, and then it must be performed in an “approved hospital”, limiting access for many. The maximum punishment for an unlawful abortion in SA? Life imprisonment.
Abortion is decriminalised in the rest of Australia – although the ACT and Queensland are the only regions to have completely removed it from the Criminal Code. Yet many women still struggle to find accessible abortion clinics and are forced to travel for an affordable and timely termination, adding weeks to their gestation and costing thousands. Women can also be denied access to an abortion or contraception due to doctors’ personal beliefs. A recent study by the University of Melbourne found that 40 per cent of rural GPs in Victoria’s west had a conscientious objection to abortion.
“Women are deluding themselves if they think we’re at a stage where we’re being treated as moral agents who have the entitlement to make decisions about our lives and bodies,” says Dr Leslie Cannold, founding director of Reproductive Choice Australia. “We’re just not there yet.”
When the law continues to criminalise abortion, it embeds stigma and allows people and institutions who oppose it to find loopholes to prevent women accessing it. “It allows healthcare providers that want to avoid providing [abortions] a way to duck their obligations on the grounds that it’s unlawful,” Cannold says. But more than that, she adds, having unequal laws that penalise women is a matter of simple inequality. “It’s also about women’s dignity. Why should this healthcare procedure, one of the safest and most common in the world but required only by women to enable them to function as full citizens, be stigmatised in this way? If we cannot control our bodies we control nothing.”
Anita-Lea Collins, a 28-year-old mother of three from regional Queensland, knows with absolute certainty that she is done having children. Not only were each of her pregnancies emotionally and physically difficult, but she simply knows her three kids are all she wants. Having decided on sterilisation, and with a referral and support from her midwife and GP, she waited five months for an appointment to see the only specialist in her town qualified to perform a tubal ligation in the public system. “Within five minutes he had refused to give me the procedure,” Collins says. “He had already decided that I would regret it and want more kids later.” Collins was adamant, but the male specialist argued back just as hard. “He said things like, ‘What if you meet a man later in life who wants your children?’” she remembers. “I said, ‘Sure, they can have children. Just not from me.’ He made me feel like my only value was for breeding purposes.” Collins says the doctor then went on to offer her other contraceptive options such as the pill and an IUD, forcing her to explain that two of her children were conceived while she was taking impermanent contraception. “I felt like he was treating me like an idiot,” Collins says. “I’m not a child. I’m a grown woman. And I know what I want. It feels really wrong and unfair that we don’t have a say on our own bodies.”
The only option for Collins now is to go down a private route – something she will struggle to afford. Around the same time that Collins was trying to get her tubes tied, another woman across the country was also attempting to take control of her own reproductive freedom. Angela Williamson, a 39-year-old mother of three, is educated, employed and lives in Hobart, Tasmania, a state where abortion has been decriminalised since 2013. When she became pregnant earlier this year, Williamson thought the most difficult part of the process would be working out what to do. “I was really surprised that the decision [to terminate] wasn’t the hardest part of it,” she says. “The hardest part was actually trying to find a doctor who could provide access to the procedure.”
To say that Williamson had to jump through hoops to access her termination is an understatement. First, she did what most women would do in 2018 – she turned to Google. “I looked at health websites in Tassie and they didn’t tell me a thing. They were full of legal terms and didn’t offer any real insight about what I should do,” she says. She went to her GP and was astonished to find she didn’t know what the options were either. As the weeks ticked by, Williamson tried a private obstetrician, who said he could perform the procedure for $2500. It was outside her budget. She tried the public Royal Hobart Hospital, but they were fully booked until after Williamson would have been 16 weeks pregnant, which would mean the hospital would need two doctors’ signatures – something they weren’t certain they would be able to secure. A representative from the hospital even called Williamson’s GP and asked if she had considered adoption. “I reached the stage where I was becoming desperate,” Williamson remembers. “It was dominating my thoughts. I needed to work. I needed to be a mum. I needed to move on. The only option left to Williamson was to book a termination with a Melbourne branch of family planning organisation Marie Stopes. Countless complications with flights, consultations and accommodation followed until she was finally able to have the procedure when she was 18 weeks pregnant. In total, including all the testing and doctor visits in Tasmania and Victoria, the experience ended up costing Williamson more than $4000.
Emotionally, it cost her even more. “I’m a confident, educated and able woman,” she wrote in her diary as she waited for the procedure in Melbourne. “Yet, I’m sitting here feeling beyond vulnerable, I’m feeling less of a person. I’m feeling invisible. I’m feeling alone. I’m feeling ashamed.” The difficulty she faced in accessing this straightforward, safe procedure in her home state had made her feel as if she had done something wrong. In contrast, the professionalism and kindness she received at the private clinic in Melbourne made Williamson realise that this should be the experience for all Australian women who want a termination. “It’s the counselling, the care, the discretion, the privacy, the security,” she says – factors that made all the difference. The Tasmanian state government has pledged to open a low-cost clinic, but Williamson’s story is reflective of the experiences many women across Australia face, where access to basic procedures is limited. According to Marie Stopes, the number of women travelling interstate for abortions increased 22 per cent from 2016 to 2017, with the majority travelling from NSW and the ACT.

“Women in rural and remote areas definitely are disadvantaged when it comes to reproductive health,” says Marie Stopes senior medical officer, Dr Catriona Melville. “If you live in a very small town, there are likely to be less medical services. And in some rural towns, particularly in conservative areas, we get very old-fashioned views, where some medical practitioners are not keen to prescribe certain contraceptives.” She says she recently spoke to a woman who was a 16-hour drive away from a large city, which is where she would have to go to access reproductive services. Then there’s the cost. Surgical abortions in Australia cost between $350 and $1500 depending on a woman’s location and the length of her gestation.
Conscientious objection by doctors is even more complicated. Laws exist all over the world, including Australia, that exempt doctors from having to perform abortions or prescribe contraception if it violates their personal views, but almost all add a caveat that insists the doctor must refer a woman to someone who will treat her. In Victoria, for example, the law says a practitioner “must refer the woman to another registered health practitioner who does not have a conscientious objection to abortion”.
And yet we know that this often doesn’t happen. Anecdotal reports suggest many doctors who object to abortion or contraception on moral grounds either refuse to refer at all, or may refer patients to anti-abortion clinics. Sometimes, the doctor’s personal objection may be disguised as medical concern. “I know many stories of doctors telling a woman that, ‘Oh, the pill is too dangerous’ or ‘No, I wouldn’t recommend you have an IUD,’” says Professor Caroline de Costa, a fellow at The Royal Australian and New Zealand College of Obstetricians and Gynaecologists. She adds that if a woman feels the doctor is not helping her find contraception, refusing to perform an abortion and not referring her in a timely manner to someone who will, then she has a right to report them to the Australian Health Practitioner Regulation Agency or the Australian Medical Association. “Both bodies would take a complaint like that very seriously,” she says.
It’s easy to think that women have bigger fights to fight, bigger wrongs to right, says Angela Williamson, who was fired from her job with Cricket Australia after tweeting from her personal account about her struggles to access abortion in Tasmania. She successfully sued her former employer for unfair dismissal and was awarded undisclosed damages. Now she plans to campaign for reproductive equality across Australia. “It is a really big deal,” she says. “Fifty-one per cent of the population are women. Reproductive freedom is a basic right.”
“[Reproductive equality] is a litmus test for whether or not a country has gender equality,” adds Leslie Cannold. “When you see laws that allow women to make their own decisions for themselves, that’s when you know you’re in a gender- equitable society. Anything else is stigmatising and insulting.”
This article appeared in this month’s February issue of Marie Claire. On sale now.










