Fast weight loss. Loss of hunger. Weight loss surgery without having to go under the knife.” Before injecting herself with Ozempic, 30-year-old Melburnian Rose never saw any negative stories about the drug touted as a weight-loss “magic bullet”. On TikTok, where the hashtag for Ozempic currently clocks in at more than 995 million views, the testimonials were positive and uplifting.
It filled Rose with hope. Having struggled with binge eating her whole life, as well as being diagnosed with an autoimmune disease, the stay-at-home mum says she had always had an issue with weight. “But with two pregnancies – stillborn twins and a healthy two-year-old – plus the longest lockdown in the world, I really lost control of the number on the scales,” she tells marie claire.
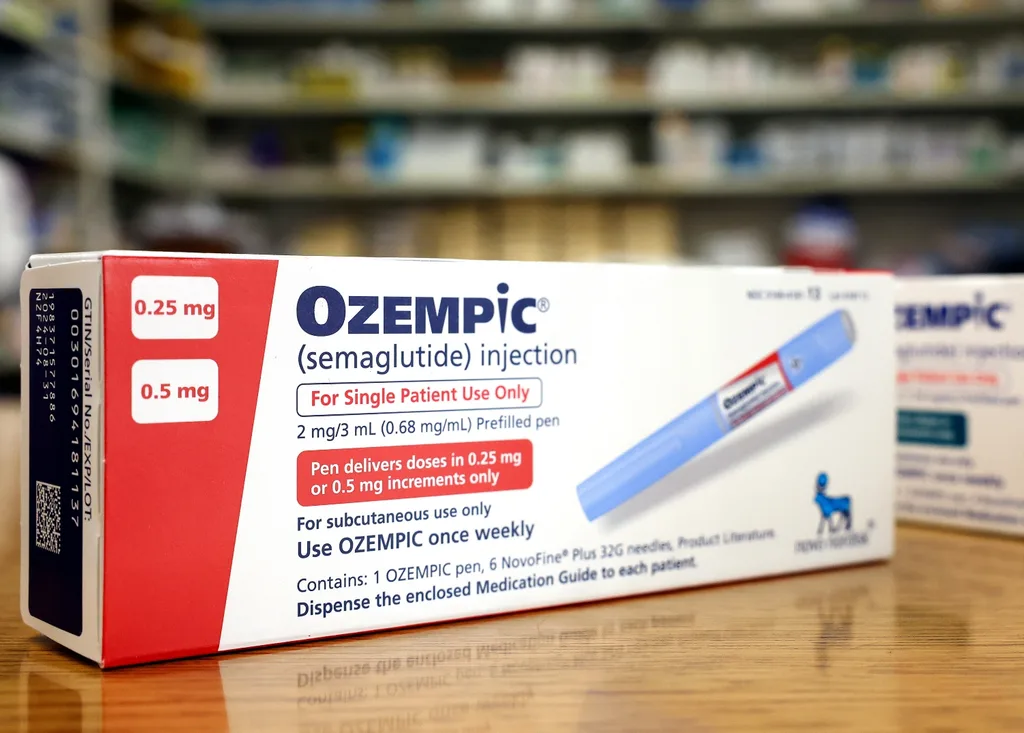
So in June last year she started taking Ozempic. Created by Danish pharmaceutical company Novo Nordisk, Ozempic is the brand name for the drug semaglutide, which is used to treat type 2 diabetes by lowering blood glucose levels. Semaglutide acts to increase the secretion of insulin from the pancreas and slows the rate at which food leaves the stomach and enters the intestine. It also slows the process of that food being absorbed in the intestine, which in turn reduces blood sugar.
“In addition, semaglutide stimulates the brain’s GLP-1 receptors, whose job it is to tell you that you’re full and you don’t need to eat anymore,” explains Professor Michael Cowley, chairman of Monash University’s Department of Physiology and former director of the Monash Obesity and Diabetes Institute. “So basically, it decreases appetite.”
Diabetic drug with a side of weight-loss, anyone? It is this side effect of the drug that has seen the proliferation of what are known as “off-label” prescriptions for the treatment of obesity and weight loss.
Dr Andrew Thompson, medical director for online clinic InstantScripts and who also heads up the company’s weight-loss program, says he has seen a marked increase in requests from people asking about semaglutide, particularly towards the end of last year. “It is probably one of the most common questions we get asked about weight loss,” he says. “Patients are aware this medication is available and it has been shown to be effective.”
Such patients include Rose. For her, the weekly injection of semaglutide was meant to be life-altering. And it was – only not the way she had hoped. “I was very unwell. The symptoms started mostly in the second week. I was dizzy, lightheaded. My eyes were blurry,” she says, ticking off the symptoms. “I had vertigo, fatigue, horrible insomnia. Nausea all day, every day.”
One of the worst symptoms was gastroparesis (paralysis of the stomach). This meant Rose wasn’t digesting food normally and would throw up what she had eaten two or three days before. Most mornings she’d vomit up a whole heap of bile. She also suffered from intense stomach pain, heartburn and reflux. The content creator, who goes by the handle “recreatingrose” on TikTok, was so sick during that time she couldn’t drive or even leave the house. Although she stopped taking the drug after only two weeks, she continued to feel the effects months later.
“I remember saying to my husband that I almost felt drugged because I was so exhausted but no matter what I did I couldn’t rest or sleep because of all the discomfort,” she says. “I also had a toddler to take care of, so I really struggled. I felt like a zombie for a whole month after my last injection. Gastroparesis is a very serious illness and to brush this off as a side effect is mind-blowing to me. Your gut truly does hold so much power and I believe this medication could really impact other aspects of your health, even though you successfully lose weight.”
Despite vowing to never take the drug again because of her negative experience, and regretting taking it in the first place, Rose makes no judgement on those who choose to use the drug. “It has had many benefits for many people,” she acknowledges.
And that’s the simple truth. Overwhelmingly, semaglutide succeeds at its primary purpose: to lower blood sugar in diabetes sufferers. With diabetes being the fastest growing chronic disease in Australia – one Australian gets diagnosed every five minutes – the benefits of semaglutide cannot be understated.
“Ozempic has just been the best thing ever for me,” 58-year-old Sydneysider Yvonne Appleby tells marie claire. The receptionist and early childhood educator first took semaglutide for her type 2 diabetes in August 2021 and couldn’t believe how great she felt.
A negative side effect of the drug was “terrible nightmares” but these disappeared after a few weeks. “I had a blood test a couple months ago and my GP was so happy because my blood glucose levels had gone right down to the normal range,” she says. “All my vitamin levels were fine. It had a positive effect on my cholesterol levels. I was actually clinically the healthiest I’ve been since I’ve been seeing my doctor. You’re basically taking this medication to lower your blood glucose level but it has many other positive side effects. Which is part of the problem right now because so many diabetes patients can’t get hold of it.”
That’s because we’re in the midst of a worldwide shortage. Although the Therapeutic Goods Administration (TGA) has advised that “limited Ozempic stock is starting to arrive in Australia” and Novo Nordisk has stated that there will be “limited and intermittent availability until June 2023”, supply is trickling through slowly and Yvonne is understandably worried.
“I’m glad it’s coming back but I know it’s been a massive problem for a lot of people who really need it and haven’t been able to get it because of the shortage,” she says. “It’s really difficult because, like me, it’s the only thing they can take. I’m actually not taking my full dose right now because … I don’t know when exactly the supply will be back. I don’t want to use it all up now and find that I have to stay off it again for a few months.”
Diabetes Australia’s Associate Professor Sof Andrikopoulos stresses the importance of patients being able to source semaglutide. “With the shortage, if people with type 2 diabetes are unable to access this medication, then their blood glucose levels are not managed,” he tells marie claire.
“That increases the risk of complications related to diabetes. Things like kidney disease, heart attacks, strokes, blindness, and then peripheral neuropathy, which leads to amputations, are all risks.”

The shortage has created tension between those suffering from diabetes and those with obesity. “I do understand obesity is a huge problem and I am not minimising that at all,” says Yvonne. “But my feeling is that Ozempic has been manufactured specifically for people with type 2 diabetes to help with their blood glucose levels and because it is specifically for that, people with type 2 diabetes should be prioritised … I know there are other diabetic medications, but a lot of them don’t work or have massive side effects. This is why [semaglutide] has been such a game changer for us.”
Novo Nordisk’s other semaglutide drug, Wegovy, could potentially help reduce the reliance on Ozempic. It is approved by the TGA to specifically treat obesity or for patients who are overweight and have comorbidities (diseases caused by obesity). It is available in the US but has yet to launch in Australia and there’s no clear indication of when that will be.
“Obesity is a serious, chronic, relapsing condition with a high prevalence and a substantial unmet medical need. We understand there is a significant need for medical treatment options for obesity,” a Novo Nordisk spokesperson tells marie claire. “We are working hard to make Wegovy available for patients living with obesity as soon as possible. The timing of its availability in Australia is not yet confirmed.”
With demand outstripping supply, other drugs are hitting the market. Pharmaceutical company Eli Lilly has a diabetes medication, Mounjaro, which works much the same way as semaglutide and has recently been approved by the TGA.
It is not yet available here. According to Cowley, Novo Nordisk is also developing a combination drug, with early dTata suggesting it can assist in weight loss of up to 28 per cent. That’s nearly a third of a person’s body weight.
Turn on the television during prime time in the US and you’ll be inundated with ads for semaglutide products. Read American magazines and it’s clear that people who are neither diabetic nor anywhere close to obese or overweight are able to get hold of the medication; privilege pays dividends.
Take the New York subway and you’ll see posters unabashedly promoting “a weekly shot to lose weight”, with close-ups of people injecting themselves. The message is in your face: thin is in. It always was and always will be.
Even though the messaging is not as conspicuous in Australia – it is illegal for companies to advertise prescription medicines directly to consumers – that doesn’t mean the discourse here around weight loss and beauty standards
is any less ugly. For all the progress made in terms of body positivity and acceptance of all body shapes, the clamour for semaglutide is evidence there’s a long way to go.

But how did Ozempic become the face of the weight-loss fix in the first place? Why is it suddenly the buzzword, considering it was approved for use by America’s Food and Drug Administration (FDA) in 2017 and by the TGA in 2019?
The answer lies with Kim Kardashian. In May last year, the whispers about Ozempic rose to a roar when the reality TV star slash businesswoman slash law student showed up wearing Marilyn Monroe’s iconic “Happy Birthday Mr President” dress at the Met Gala.
Despite saying she went on a restrictive diet to fit into the dress, speculation was rife that she had taken the weight-loss drug. Rumours flew about several other celebrities and reality TV stars who had lost weight or became notably slimmer.

Some, such as The Real Housewives of Beverly Hills star Kyle Richards, denied it. Others, such as American comedian Chelsea Handler and model Remi Bader, did not, although Handler admitted to taking it accidentally and Bader discouraged others from taking the drug if it was not medically required.
Thompson warns against the drug being referred to as a “magic bullet” for weight loss. “Weight management is a very complex issue,” he says. “The critical thing is that weight loss is not about taking medication. It’s about a lifestyle adjustment, as well as adjusting our psycho-social environment and our relationship to our body and our weight.
It’s about getting a healthier appreciation for oneself, so we can develop strategies for that patient to move forward. No medication is a magic bullet. That is a complete fallacy. These medications will help with the journey for these patients but they will definitely not be a one-size-fits-all solution.”
There is also a big question mark around whether the drug is safe to take if it is not being used to treat diabetes – after all, that’s what semaglutide was made for. “We don’t know if it’s safe,” says Cowley.
“When the company tests these drugs, it tests them within a particular patient population for whom they’re seeking permission to prescribe the drug to. In patients who are not in that population, we really don’t know what’s going to happen because it’s never been tested. We can infer it is probably safe because people who have diabetes and obesity are not vastly different to those who don’t. But they are different because diabetes patients have a disease. We don’t know what the consequences will be for those who don’t have diabetes.”
What we do know is that nausea, vomiting and stomach pain are common side effects. Rose from Melbourne can attest to that. Some people also complain of “Ozempic face”, a term used to describe premature ageing because of facial skin sagging.
There are also rare side effects such as pancreatitis, which can be fatal. Given her own experience with semaglutide, Rose wants people to think of the drug as a last option, rather than the first solution.
“I remember visiting the ER a few months after [taking the drug] with unrelated abdominal pain,” she says. “The ER doctor asked me if I had tried any new meds. I mentioned I was on Ozempic months earlier and she told me that they were seeing a huge number of patients suffering from illness while being on this medication but also so many posts faking it. Things like kidney and liver problems, gallstones and paralysed stomachs. I was shocked. I think it’s important for people to understand how serious this medicine is.”
Having a daughter has made Rose even more aware of how society talks about weight and body image. She doesn’t want her child to grow up with impossible beauty standards. “I wanted to share a raw and unsuccessful experience with this ‘wonder drug’ because it seems all of its dangers are being pushed under the rug,” she says. “They say nothing tastes as good as skinny feels, but at what risk? This mindset is outdated and it’s wild that Hollywood is going down that path again. A healthy and happy body and mind is something we should all strive towards. There is no baseline for that.”
This story originally appeared in the July issue of marie claire.










